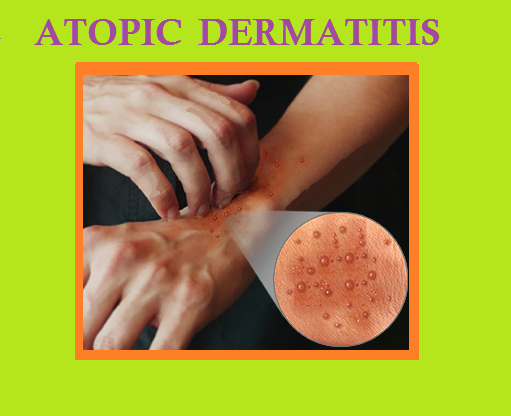
ATOPIC DERMATITIS
Atopic dermatitis looks different at different ages and in people of different races. Diagnostic criteria for atopic dermatitis must include pruritus, typical morphology and distribution (flexural lichenification, hand eczema, nipple eczema, and eyelid eczema in adults), onset in childhood, and chronicity.
In diagnosing the disease following points should also be considered like personal or family history of atopic disease (asthma, allergic rhinitis, atopic dermatitis), xerosis-chthyosis, facial pallor with infraorbital darkening, elevated serum IgE, and repeated skin infections.
SYMPTOMS
Itching may be severe and prolonged. Rough plaques without the thick scale and discrete demarcation of psoriasis affect mainly the neck, trunk and face. The flexural skin of elbows and knees are involved. In chronic cases of atopic dermatitis, the skin is dry, leathery, and lichenified. In black patients with severe disease, pigmentation may lost in lichenified areas. In acute flares, widespread be redness with weeping, may be diffusely or in discrete plaques may be happened.
DIAGNOSIS
Atopic dermatitis must be distinguished from seborrheic dermatitis (less pruritic, frequent scalp and face involvement, and scaly lesions). Secondary staphylococcal infections may exacerbate atopic dermatitis, and should be considered during hyperacute, weepy flares of atopic dermatitis. Fissuring where the earlobe connects to the neck is a cardinal sign of secondary infection.
TREATMENT
Atopic patients have hyperirritable skin. Anything that dries or irritates the skin will potentially trigger dermatitis. Atopic individuals are sensitive to low humidity and often get worse in the winter. Adults with atopic disorders should not bathe more than once daily Soap should be confined to the armpits groin, scalp, and feet. Washcloths and brushes should not be used. After rinsing, the skin should be patted dry (not rubbed) and then immediately-within three minutes- covered with a thin film of an emollient such as Aquaphor, Eucerin, petrolatum, Vanicream, or a corticosteroid as needed. Vanicream can be used if contact dermatitis resulting from additives in medication is suspected. Atopic patients may avoided wools and acrylics. Cottons are preferable, but synthetic blends also are considered. Other triggers of eczema in some patients include sweating, ointments and heat.
Local Treatment
Corticosteroids should be applied sparingly to the dermatitis once or twice daily and rubbed in well. Their potency should be appropriate to the severity of the dermatitis. In general, one should begin with triamcinolone stronger corticosteroid then taper to hydrocortisone or another slightly stronger mild corticosteroid (alclometasone, desonide). It is vital that patients taper off corticosteroids and substitute emollients as the dermatitis clears to avoid the side effects of corticosteroids. Tapering is also important to avoid rebound flares of the dermatitis that may follow their abrupt cessation. Tacrolimus ointment and pimecrolimus cream can be effective in managing atopic dermatitis when applied twice daily. These medications do not cause skin atrophy or striae, avoiding the complications of long-term topical corticosteroid use. They are safe for application on the face and even the eyelids. Tacrolimus and pimecrolimus should be avoided in patients at high risk for lymphoma (ie, those with HIV, iatrogenic immunosuppression, prior lymphoma). The treatment of atopic dermatitis is dictated by the pattern and stage of the dermatitis-acute/weepy, sub- acute/scaly, or chronic/lichenified.
SYSTEMIC THERAPY
Systemic corticosteroids are indicated only for severe acute exacerbations. Oral prednisone dosages should be high enough to suppress the dermatitis quickly. The dosage is then tapered to nil over a period of 2-4 weeks. Owing to the chronic nature of atopic dermatitis and the side effects of chronic systemic corticosteroids, long-term use of these agents is not recommended for maintenance therapy. Fissures, crusts, erosions, or pustules indicate staphylococcal infection clinically. Anti staphylococcal antibiotics given systemically such as a first-generation cephalosporin or doxycycline if methicillin-resistant Staphylococcus aureus is suspected may be helpful. Cultures to exclude methicillin-resistant S aureus are recommended. However, in this setting, continuing and augmenting the topical anti-inflammatory treatment often improves the dermatitis, despite the presence of infection. Phototherapy can be an important adjunct for severely affected patients, and the properly selected patient with recalcitrant disease may benefit greatly from therapy with UVB with or without coal tar or PUVA (psoralen plus ultraviolet A). Oral cyclosporine, mycophenolate mofetil, methotrexate, or azathioprine may be used for the most severe and cases
COMPLICATION OF TREATMENT
The patients should be monitored for skin atrophy. Eczema herpeticum, a generalized herpes simplex infection manifested by monomorphic vesicles, crusts, or scalloped erosions superimposed on atopic dermatitis or other extensive eczematous processes, is treated successfully with oral acyclovir, or intravenous acyclovir. Smallpox vaccination is absolutely contraindicated in patients with atopic dermatitis or a history there of because of the risk of eczema vaccinatum (wide- spread vaccinia infection, preferentially in areas of dermatitis).
Atopic dermatitis runs a chronic or intermittent course. Affected adults may have only hand dermatitis. Poor prognostic factors for persistence into adulthood in atopic dermatitis include onset early in childhood, early generalized disease, and asthma.
For Informational purpose only. Consult your Physician for advice.